Fortaleciendo la experticia adaptativa en la educación quirúrgica: un enfoque integral y estratégico
DOI:
https://doi.org/10.30944/20117582.2477Palabras clave:
competencia profesional, metacognición, aprendizaje profundo, apoyo a la formación profesional, educación de postgrado en medicina, cirugía generalResumen
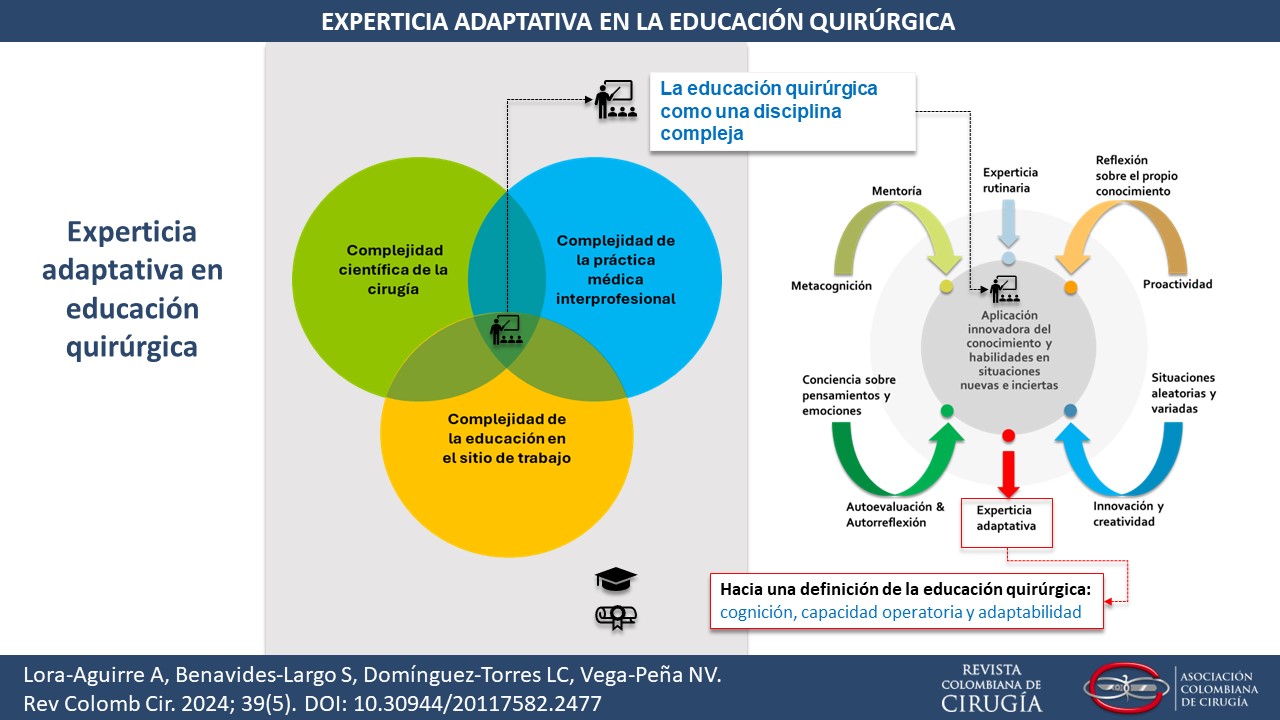
Introducción. La formación integral de los residentes excede el conocimiento teórico y la técnica operatoria. Frente a la complejidad de la cirugía moderna, su incertidumbre y dinamismo, es necesario redefinir la comprensión de la educación quirúrgica y promover capacidades adaptativas en los futuros cirujanos para manejar efectivamente el entorno. Estos aspectos se refieren a la experticia adaptativa.
Métodos. La presente revisión narrativa propone una definición de la educación quirúrgica con énfasis en la experticia adaptativa, y un enfoque para su adopción en la práctica.
Resultados. Con base en la literatura disponible, la educación quirúrgica representa un proceso dinámico que se sitúa en la intersección de la complejidad de la cultura quirúrgica, del aprendizaje en el sitio de trabajo y de la calidad en el cuidado de la salud, dirigido a la formación de capacidades cognitivas, manuales y adaptativas en el futuro cirujano, que le permitan proveer cuidado de alto valor en un sistema de trabajo colectivo, mientras se fortalece su identidad profesional. La experticia adaptativa del residente es una capacidad fundamental para maximizar su desempeño frente a estas características de la educación quirúrgica. En la literatura disponible se encuentran seis estrategias para fortalecer esta capacidad.
Conclusión. La experticia adaptativa es una capacidad esperada y necesaria en el médico residente de cirugía, para hacer frente a la complejidad de la educación quirúrgica. Existen estrategias prácticas que pueden ayudar a fortalecerla, las cuales deben ser evaluadas en nuevos estudios.
Descargas
Referencias bibliográficas
Doll WE, Trueit D. Complexity and the health care professions. J Eval Clin Pract. 2010;16:841-8. https//doi.org/10.1111/j.1365-2753.2010.01497.x
Cilliers P. Understanding complex systems. En: Sturmberg JP, Martin CM, editors. Handbook of systems and complexity in health. London: Springer; 2013. p. 27-38. https://doi.org/10.1007/978-1-4614-4998-0
Norman G. Chaos, complexity and complicatedness: Lessons from rocket science. Med Educ. 2011;45:549-59. https://doi.org/10.1111/j.1365-2923.2011.03945.x
Woodruff JN. Accounting for complexity in medical education: A model of adaptive behaviour in medicine. Med Educ. 2019;53:861-73. https://doi.org/10.1111/medu.13905
Patiño JF. Las teorías de caos y de complejidad en cirugía. Rev Colomb Cir. 2000;15:209-13.
Rickles D, Hawe P, Shiell A. A simple guide to chaos and complexity. J Epidemiol Community Health. 2007;61:933-7. https://doi.org/10.1136/jech.2006.054254
Waldrop MM. Complexity: The emerging science at the edge of order and chaos. New York: Simon & Schuster; 1992. 384 p.
Lewin R. Complexity: Life at the edge of chaos. Chicago: University of Chicago Press; 2000. 242 p.
Mennin S. Complexity and health professions education: A basic glossary. J Eval Clin Pract. 2010;16:838-40. https://doi.org/10.1111/j.1365-2753.2010.01503.x
Cameron KS, Quinn RE. Diagnosing and changing organizational culture: Based on the competing values framework. Revised edition. San Francisco: Jossey-Bass; 2011. 205 p.
Kerr B, O’Leary JP. The training of the surgeon: Dr. Halsted’s greatest legacy. Am Surg. 1999;65:1101-2.
Schlich T. Introduction: What is special about the history of surgery? En: Schlich T, ed. The Palgrave handbook of the history of surgery. London (UK): Palgrave Macmillan; 2017. p. 1-26.
Hill E, Bowman K, Stalmeijer R, Hart J. You’ve got to know the rules to play the game: How medical students negotiate the hidden curriculum of surgical careers. Med Educ. 2014;48:884-94. https://doi.org/10.1111/medu.12488
Schlich T. ‘The days of brilliancy are past’: Skill, styles and the changing rules of surgical performance, ca. 1820-1920. Med Hist. 2015;59:379-403. https://doi.org/10.1017/mdh.2015.26
Arnold-Forster A. The social and emotional world of twentieth-century anglo-american surgery: The James IV Association of Surgeons. Bull Hist Med. 2022;96:71- 101. https://doi.org/10.1353/bhm.2022.0002
Luu S, Leung SOA, Moulton CA. When bad things happen to good surgeons: Reactions to adverse events. Surg Clin North Am. 2012;92:153-61. https://doi.org/10.1016/j.suc.2011.12.002
Martinez W, Lehmann LS. The “hidden curriculum” and residents’ attitudes about medical error disclosure: Comparison of surgical and nonsurgical residents. J Am Coll Surg. 2013;217:1145-50. https://doi.org/10.1016/j.jamcollsurg.2013.07.391
Gkiousias V. Scalpel please! A scoping review dissecting the factors and influences on professional identity development of trainees within surgical programs. Cureus. 2021;13:e20105. https://doi.org/10.7759/cureus.20105
Quintana-Montejo N, Vega-Peña NV, Domínguez-Torres LC. Knowledge-building in surgery: An evolving craft. Cir Esp (Engl Ed). 2023;101:565-9. https://doi.org/10.1016/j.cireng.2023.02.008
Brandt ML. Sustaining a career in surgery. Am J Surg. 2017;214:707-14. https://doi.org/10.1016/j.amjsurg.2017.06.022
Norcini J, Talati J. Assessment, surgeon, and society. Int J Surg. 2009;7:313-7. https://doi.org/10.1016/j.ijsu.2009.06.011
Sachdeva AK, Blair PG, Lupi LK. Education and training to address specific needs during the career progression of surgeons. Surg Clin North Am. 2016;96:115-28. https://doi.org/10.1016/j.suc.2015.09.008
Lovell B. ‘We are a tight community’: Social groups and social identity in medical undergraduates. Med Educ. 2015;49:1016-27. https://doi.org/10.1111/medu.12781
Himidan S, Kim P. The evolving identity, capacity, and capability of the future surgeon. Semin Pediatr Surg. 2015;24:145-9. https://doi.org/10.1053/j.sempedsurg.2015.02.015
Mitchell T. Adapting for the future: Flexibility of UK postgraduate training. Surgery (Oxf). 2020;38:670-4. https://doi.org/10.1016/j.mpsur.2020.07.004
Bates J, Ellaway RH. Mapping the dark matter of context: A conceptual scoping review. Med Educ. 2016;50:807- 16. https://doi.org/10.1111/medu.13034
Sfard A. On two metaphors for learning and the dangers of choosing just one. Educational Researcher. 1998;27:4-13. http://dx.doi.org/10.2307/1176193
Billet S. Understanding workplace learning: Cognitive and sociocultural perspectives. En: Boud D, ed. Current issues and new agendas in workplace learning. Leabrook: National Centre for Vocational Education Research Ltd. - NCVER; 2003. p. 43-59.
Hager P. Theories of work, place and learning. En: Malloch M, Cairns L, Evans K, O’Connor BN, editors. The SAGE handbook of workplace learning. London: SAGE; 2011. p. 17-31.
Elrod JK, Fortenberry JL. Centers of excellence in healthcare institutions: What they are and how to assemble them. BMC Health Serv Res. 2017;17(Suppl 1):425. https://doi.org/10.1186/s12913-017-2340-y
Mylopoulos M, Farhat W. “I can do better”: Exploring purposeful improvement in daily clinical work. Adv in Health Sci Educ. 2015;20:371-83. https://doi.org/10.1007/s10459-014-9533-5
Hanefeld J, Powell-Jackson T, Balabanova D. Understanding and measuring quality of care: dealing with complexity. Bull World Health Organ. 2017;95:368-74. https://doi.org/10.2471/BLT.16.179309
Engeström Y. Expertise in transition: Axpansive learning in medical work. UK: Cambridge University Press; 2018. 283 p.
Pusic MV, Hall E, Billings H, Branzetti J, Hopson LR, Regan L, et al. Educating for adaptive expertise: case examples along the medical education continuum. Adv in Health Sci Educ. 2022;27:1383-400. https://doi.org/10.1007/s10459-022-10165-z
Pelgrim E, Hissink E, Bus L, van der Schaaf M, Nieuwenhuis L, van Tartwijk J, et al. Professionals’ adaptive expertise and adaptive performance in educational and workplace settings: An overview of reviews. Adv in Health Sci Educ. 2022;27:1245-63. https://doi.org/10.1007/s10459-022-10190-y
Cheung JJH, Kulasegaram KM. Beyond the tensions within transfer theories: Implications for adaptive expertise in the health professions. Adv in Health Sci Educ. 2022;27:1293-315. https://doi.org/10.1007/s10459-022-10174-y
Kua J, Lim WS, Teo W, Edwards RA. A scoping review of adaptive expertise in education. Med Teach. 2021;43:347-55. https://doi.org/10.1080/0142159X.2020.1851020
Croskerry P. Adaptive expertise in medical decision making. Med Teach. 2018;40:803-8. https://doi.org/10.1080/0142159X.2018.1484898
Pusic MV, Santen SA, Dekhtyar M, Poncelet AN, Roberts NK, Wilson-Delfosse AL, et al. Learning to balance efficiency and innovation for optimal adaptive expertise. Med Teach. 2018;40:820-7. https://doi.org/10.1080/0142159X.2018.1485887
Steinert Y, Irby DM, Dolmans D. Reframing faculty development practice and research through the lens of adaptive expertise. Med Teach. 2021;43:865-7. https://doi.org/10.1080/0142159X.2021.1931081
Ferguson JH, Lehmann J, Zastavker YV, Chang S, Higginson RP, Talgar CP. Adaptive expertise: The development of a measurement instrument. En: ASEE Annual Conference and Exposition, Conference Proceedings. American Society for Engineering Education; 2018. Disponible en: https://peer.asee.org/adaptive-expertise-the-development-of-a-measurement-instrument
Grunefeld H, Prins FJ, van Tartwijk J, Wubbels T. Development of educational leaders’ adaptive expertise in a professional development programme. International Journal for Academic Development. 2022;27:58-70. https://doi.org/10.1080/1360144X.2021.1898966
Domínguez LC, Dolmans D, Restrepo J, de Grave W, Sanabria A, Stassen L. How surgical leaders transform their residents to craft their jobs: Surgeons’ perspective. J Surg Res. 2021;265:233-44. https://doi.org/10.1016/j.jss.2021.03.034
Dominguez LC, Dolmans D, de Grave W, Donkers J, Sanabria A, Stassen L. Supervisors’ transformational leadership style and residents’ job crafting in surgical training: The residents’ views. Int J Med Educ. 2022;13:74-83. https://doi.org/10.5116/ijme.622d.e2f6
Mylopoulos M, Steenhof N, Kaushal A, Woods NN. Twelve tips for designing curricula that support the development of adaptive expertise. Med Teach. 2018;40:850-4. https://doi.org/10.1080/0142159X.2018.1484082
Jensen RD, Brydges R, Grierson L. Re-examining the integration of routine and adaptive expertise: There is no such thing as routine from a motor control perspective. Adv in Health Sci Educ. 2022;27:1283-91. https://doi.org/10.1007/s10459-022-10163-1
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2024 Revista Colombiana de Cirugía

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
Todos los textos incluidos en la Revista Colombiana de Cirugía están protegidos por derechos de autor. Las opiniones expresadas en los artículos firmados son las de los autores y no coinciden necesariamente con las de los directores o los editores de la Revista Colombiana de Cirugía. Las sugerencias diagnósticas o terapéuticas como elección de productos, dosificación y métodos de empleo corresponden a la experiencia y al criterio de los autores.
















.jpg)